Oral health and other diseases
Your mouth is the gateway to your body
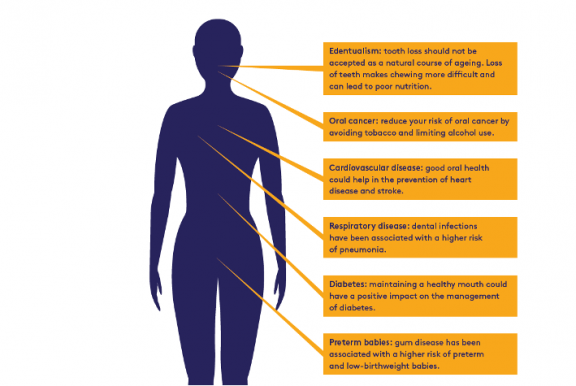
Keeping the mouth healthy is crucial for maintaining general health and well-being. If not properly managed, oral diseases can negatively impact the rest of your body and affect every aspect of life, including personal relationships, self-confidence, as well as school and work attendance, and overall performance. A healthy mouth may also help in the prevention of other health conditions, such as heart and respiratory diseases, cancer and diabetes.
Oral health is about much more than healthy teeth and a good-looking smile. The mouth is a mirror of the body, often reflecting signs of other diseases. For example, oral lesions may be the first signs of HIV-infection, and changes in tooth appearance can indicate serious eating disorders.
Globally, 38.0 million people were estimated to live with HIV at the end of 20191. First signs of HIV infection often appear in the mouth. More than half of people living with HIV develop oral symptoms at the early stage of the disease such as fungal, bacterial, and viral infections. These can all cause pain and discomfort, dry mouth, leading to difficulty in chewing, swallowing, and tasting food, which has a significant negative impact on quality of life2.
Treatment and management of HIV-related oral lesions
- HIV-related oral lesions can be used to diagnose HIV infection, monitor the disease progression, predict immune status and contribute to timely therapeutic treatment, which can considerably improve quality of life and well-being.
- Dentists and oral healthcare professionals can also ensure that patients with oral manifestations are referred for testing of HIV/AIDS and have appropriate medical follow-up.
- Early detection of HIV-related oral lesions can be used to diagnose HIV infection and monitor the disease’s progression. Early detection is also important for timely treatment.
Noncommunicable diseases (NCDs), also known as chronic diseases, are a growing global threat. NCDs are the leading cause of death and disability, killing 41 million people each year and are responsible for 71 per cent of all deaths globally, 85 per cent of which occur in low- and middle-income countries3. Oral diseases contribute significantly to the NCD burden with untreated dental caries being the most common health condition worldwide, affecting approximately 2.4 billion people and oral cancer ranked among the 10 most common cancers.
Poor oral health can be the result, as well as the cause, of poor general health. Many general conditions increase the risk of oral diseases, such as an increased risk of periodontal (gum) disease in patients with diabetes. Equally, poor oral health has been linked with a number of general health conditions and their management, including heart disease, respiratory diseases, and some cancers3.
Understand your risk and take action to prevent disease
- Most oral diseases share modifiable (you can take measures to change them) risk factors with the other NCDs, so taking action to protect your oral health can have a positive impact on your general health, well-being and quality of life.
- Oral health and general health can be maintained by being aware of your risk factors, which include an unhealthy diet high in sugar, tobacco use, harmful use of alcohol and poor oral hygiene, and taking action to prevent disease.
- Read How to maintain good oral health and Control your risk factors to understand how you can keep your mouth functioning correctly and protect your overall health.
Periodontal (gum) disease and diabetes have a two-way relationship: in general, people with diabetes have an increased risk of developing periodontal disease, and treatment of periodontal disease often improves blood glucose levels.
Moreover, there is a casual link between high consumption of sugar and diabetes, obesity and dental caries4.
Manage risk and get regular dental check-ups
- Too much sugar in the blood can lead to more sugar in saliva – this sugar then contributes to tooth decay and periodontal disease. High blood sugar levels can also harm the blood vessels in the gums, making them more likely to get infected.
- Regular dental check-ups and treatment of periodontitis (a condition that destroys tooth-supporting tissues and bone), may contribute to effective management of type 2 diabetes5.
